Setting goals
Studies suggest that people are more likely to be successful when making changes if they have set a realistic goal that is important to them. Making changes depends on the perceived balance of the pros and cons of making the change – if there are a lot of barriers and only a few benefits, change often does not happen. Removing the barriers and increasing the perceived benefits can make change more likely. Changes include increasing activity such as walking, taking the stairs, parking further from the supermarket, getting off the bus a stop early, or increasing healthy food choices such as trying lower energy/carbohydrate foods that might make food changes more palatable.
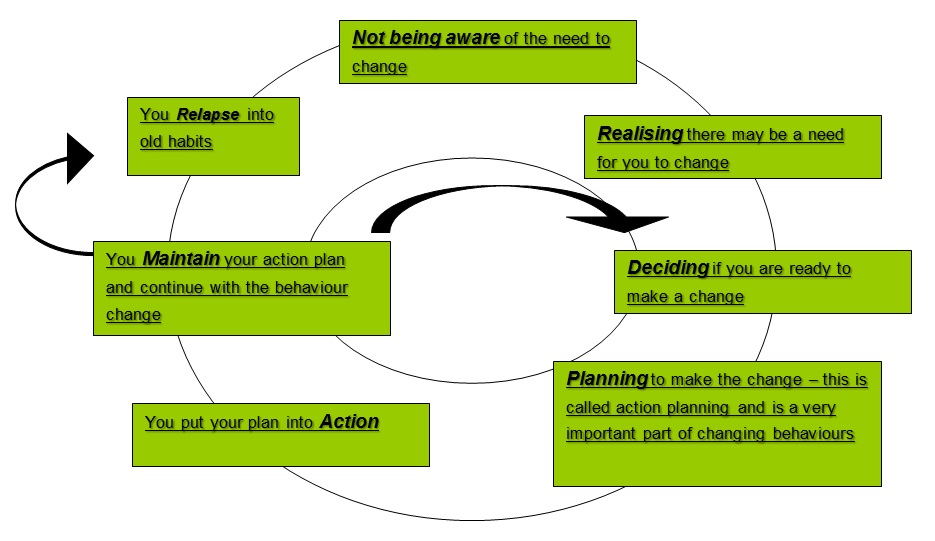
Making a change can be difficult. Some people have tried to explain behaviour change using a ‘cycle of change’:
This model suggests that a person may have something they need to change without even realising it. You may only realise that you need to change when someone says something to you about it. Once you are aware of this possible need to change, you will be trying to decide if it’s something you feel you can change now or not. If you decide it’s a good time for you to change, you would begin planning how you would make this change. This is an important step. Most people find their goals more difficult to achieve if they haven’t planned well. You are more likely to make the change sustainable if you have planned well in the first instance.
When action planning for goals, it is suggested you try to make it a behaviour that you can change. As an example we have used a “weight loss goal” using exercise as the behaviour.
- Being exact about what you are planning to do. E.g. ‘I will walk for at least 20 minutes five times a week to help with weight loss or preventing weight gain’.
- Set a plan that you can actually do. E.g. ‘I will try walking 3 times a week to begin with, and increase to 5 times a week if I feel comfortable doing so.’ Be realistic and make it achievable.
- Think about timing. E.g. I will ask a friend if they will walk with me every morning before work.
- Think about how confident you are. This is very important when making changes. If you feel this is something that you cannot change at the moment it could mean you are less likely to succeed. If you rate your confidence as less than 7 out of 10 then it may mean you are not quite ready to make this change. This will give you the chance to think about why you are not confident in making this change and will help when it comes to planning again.
- What might stop you from making this change? It might be that your friend can’t join you on one day, or it’s raining/snowing, or you don’t have the right shoes.
- Get support. You could do this by explaining to your friend how important this is to you, asking several friends to come with you on different days, buy all weather gear, etc..
There is no rule as to how frequently you set yourself new goals and develop action plans. You might find it useful to review “where you are at” every now and again. Sometimes it can be difficult to get back on track and it could be that contacting a friend or peer might be able to help give you the extra support you need.
Below we have provided three resources to help you with changing behaviour.
- The action planning document here can help you to begin to think about how to change behaviour.
- The changing behaviour document here is useful in thinking about the pros and cons with changing the behaviour.
- The goal setting document here helps you think about setting SMART goals to help change behaviour.
You might decide that certain of these documents would work better for you in your sessions – there are no rules on which one/s to use.
Problem-solving
One way to think about the challenges that people with a health condition face is to regard them as problems to be solved. This brings focus to peer support and is a good approach for those who think of themselves as ‘doers’ who like to take a practical approach to things.
Often, similar types of problems will come up in peer support. Below we have listed some common problems in diabetes peer support groups. For each one, you can think about some solutions, and then view our suggestions by clicking the arrows.
-
-
- Share your experiences with the peer, but be aware that everyone with the condition is different.
- Suggest some internet sites or hand them a relevant leaflet.
- Suggest the peer makes an appointment with their GP or other health professional.
-
- Suggest they take someone with them to their next appointment.
- Suggest they take a list of questions with them to the next appointment.
- Get them to ask the health care professional to write down their advice.
- Is unable to tolerate a medicationEncourage the peer to make an appointment with their GP or practice nurse to look at possible changes.
- Has difficulties exercising e.g. has arthritis1. Look on the internet or draw on your own personal experience to suggest some light exercise classes. 2. Suggest the peer ask their GP or practice nurse for a referral to a suitable exercise programme.
- Has a low income and struggles to afford a healthy diet1. Think about some inexpensive ways to create healthy food with the peer.
2. If getting to a supermarket is difficult, suggest using a dial-a-ride scheme or finding a car share.
3. Suggest they visit the Citizens Advice Bureau for information about their entitlements. - Finds it hard to motivate themselves to stick to their medication regimen1. Talk to them about why they think they are not motivated
2. Work through the Smart Goals and Cycle of Change with them [link to these here] 3. If the peer feels it is a serious issue, offer to refer them to a health professional. - Has unsupportive partner or family members1. Talk to the peer about the small things the partner perhaps does do and help them think of ways of building on these.
2. Suggest they make an appointment with their practice nurse, and ask the partner to attend with them. - Has a fear of needles but requires injections e.g. insulinSuggest they make an appointment with their GP about this, who can refer them to a relevant specialist to help them overcome/adapt to their fear.
- Finds it difficult to make appointments1. Get them to explain what they find difficult about their GP’s appointment system.
2. Help them make an appointment. - Feels very down or sad1. Listen with empathy
2. Encourage them to try out the Happiness Manifesto on page 50.
3. Suggest they make an appointment with their GP. - Finds it difficult to read important letters and information sheets1. Offer to read through things with them, in a patient and calm way.
2. Suggest they considering attending a local ‘skills for life’ course – it’s never too late to learn.
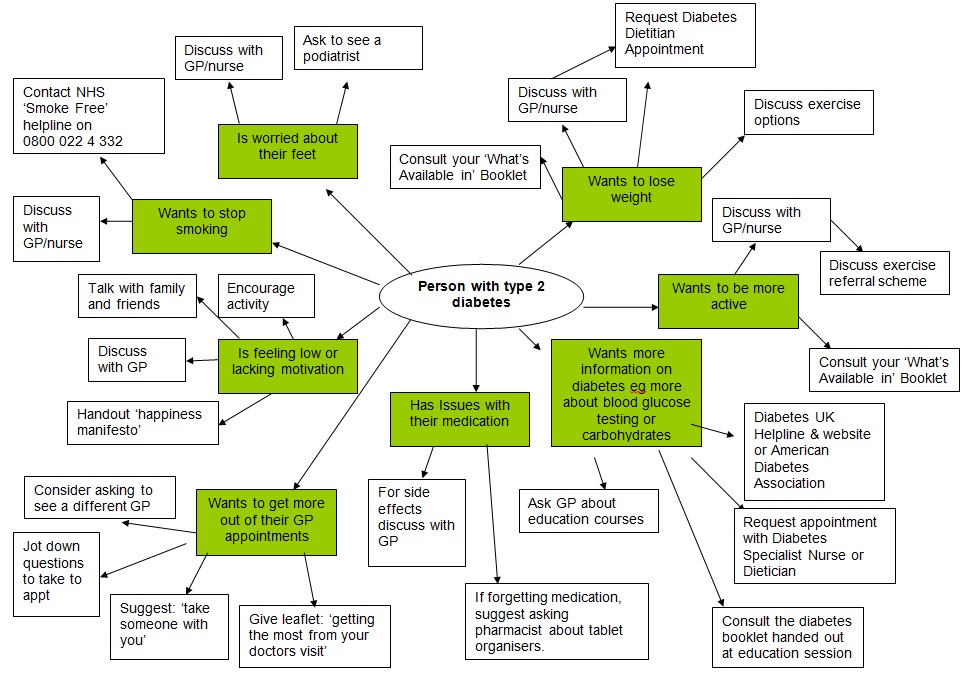
One resource that may help with problem solving is the following ‘spider’ diagram. It suggests options for various problems a peer may be facing: